Visit Vale Health Marketplace?
You are leaving balladhealth.org to visit Vale Health’s Wellness Marketplace.
Disclaimer: Ballad Health does not sponsor, endorse or recommend any product or resource listed in the marketplace.
Alan Levine, executive chairman and CEO of Ballad Health, spoke on Tuesday afternoon, Sept. 25, to a subcommittee of the United States Senate Committee on Health, Education, Labor and Pensions (HELP). The subcommittee hearing is titled “Health Care in Rural America: Examining Experiences and Costs.”
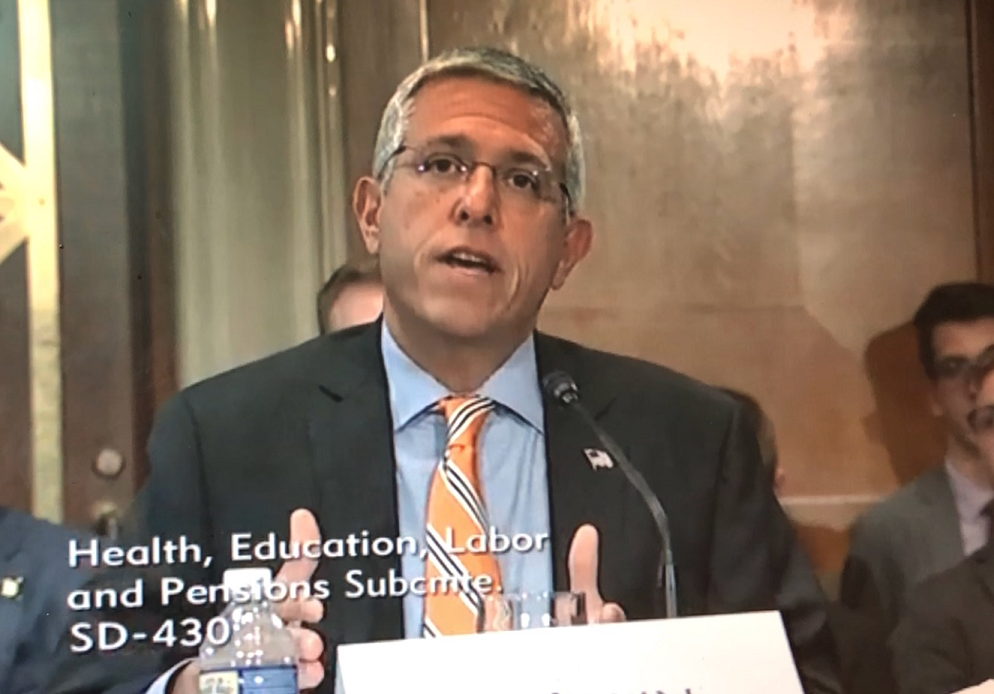
Levine’s written testimony, which was submitted to the U.S. Senate, is below. During the live hearing, he presented an oral summary outlining some of the most critical issues facing rural hospitals in the United States as well as legislative and regulatory strategies that can help communities address the health issues that disproportionately affect rural and non-urban residents throughout the country.
Levine was one of four experts speaking before the subcommittee.
You can read Levine’s full written testimony here:
Alan M. Levine
Executive Chairman, President, and Chief Executive Officer
Ballad Health
Former Secretary, Louisiana Department of Health and Florida Agency for Health Care Administration
Chairman Enzi, Chairman Alexander, Ranking Member Sanders, Ranking Member Murray, and members of the committee, thank you for the invitation and opportunity to appear before you this afternoon.
My name is Alan Levine, and I currently serve as the executive chairman, president and chief executive officer of Ballad Health, a 21-hospital, not-for-profit integrated healthcare delivery system uniquely created through state action immunity upon the merger of two regional health systems. We serve 29 counties in the Appalachian region of Upper East Tennessee, Southwest Virginia, East Kentucky, and Western North Carolina.
Thank you for inviting me to discuss the variety of healthcare challenges facing Americans in rural areas, and the concerns those of us responsible for delivering health care services have with respect to ensuring access and improving health. As the evidence shows, rural hospitals and clinics are facing unprecedented pressure. Researchers at the University of North Carolina have identified almost 90 rural hospital closures across the country in just the last eight years, and iVantage Health Analytics has reported that 673 other rural hospitals are at risk of closure due to mounting financial pressures.
These hospitals are the epicenter of most of these communities, not just for health care but for community-wide economic stability. In addition, the dated reimbursement models and brick-and-mortar approach to health care of yesterday are undermining these assets. Payment policies and well-intended policy reforms are overly sophisticated and bureaucratic. While the jury is out on whether these policies, which continue to quickly evolve, will work, it is highly likely most of the thought behind the policies is aimed at urban and higher density markets where much of the spending occurs. In my view, not enough thought has gone into how these policies weigh on smaller, non-urban and rural community assets. The fragmentation of payment and the weight of these policies undermine efforts to transition these rural assets into what is actually needed in these communities. One need look no further than the closings of hospitals, and the financial performance of the largest rural and non-urban hospital providers – both publicly traded and not-for-profit – to validate this point. We have before us a situation where it seems the only two options are: provide more funding for rural hospitals through convoluted formulas and one-size-fits-all rules, or let rural hospitals close.
I firmly believe there are options in between these two extremes which can help sustain our rural and non-urban communities.
Let’s face it. Rural economies are continuing to struggle, and are not yet enjoying the full benefit of the recovery. According to the National Rural Health Association, only three percent of the job growth that has occurred since the Great Recession has happened in rural areas, and between 2010 and 2014, more businesses closed than opened in rural areas. Today across the nation, rural and non-urban hospitals find themselves in negative feedback loops, increasingly leading to bankruptcy and closure. It starts with declining revenues caused by declining inpatient utilization rates. Combining declining inpatient use rates with stagnant or declining populations is a dangerous mix for a rural hospital or health system. Add to this mix the multitude of federal and private insurer payment policies designed to contain or even reduce per-unit reimbursement, which remains tied to the fee-for-service system, and the hospitals lose the necessary revenue to service fixed costs. These hospitals have also amassed debt they must service, and the ongoing fixed costs of operating a hospital continue to grow. If the variable margins decline, the financial model simply does not work. Then, add to this scenario the highly complex changes being imposed by Medicare and Medicaid, and the cost of compliance, and you are left with hospitals that simply don’t have a chance, particularly if they are not part of a larger health system. But even if they are part of a larger system, those same policies that undermine the financial health of the larger regional non-urban hospitals is beginning to lead to decisions to close or alter the relationships with rural hospitals. This very instance is playing out today in West Tennessee, where a regional not-for-profit system acquired a rural hospital, and closed it. The process of failure is familiar to us all. Inability to service fixed costs translates into reduced cash flow, which negatively impacts employee and physician recruitment and retention, reduced investment into capital assets like newer equipment and technology, and eventually the decline of the physical structure itself.
As these investments deteriorate, patients with means (and commercial insurance) travel to urban and suburban hospitals for orthopedic, cardiovascular and other procedures, which our current reimbursement system disproportionately rewards with higher margins. These margins are used by hospitals to offset losses in most other service lines of a hospital. Rural hospitals are thus left with a less-favorable case mix and payor mix, leading to further declines in revenue and margin.
This is the death spiral.
But, as I have stated, these hospitals don’t have to close. There is another option. Transitioning these hospitals to what is needed today can be financially beneficial and can serve a major public health policy purpose. Today’s rural hospital does not need to be providing high acuity intensive services or high acuity surgeries. Indeed, it may be better for patients to go to larger regional facilities that sustain the volume necessary to provide high quality intensive services. But, since 97 percent of our nation’s land area is rural, access to many needed services is hampered by geography – this is geography that rural hospitals can help serve where serious service gaps exist. By building a bridge from yesterday’s fee-for-service, brick-and-mortar model focused on payment for each inpatient encounter or surgery to one where rural hospitals become the epicenter for the evolved needs of mental health, addiction services, primary care, chronic care for certain chronic conditions, obstetrics and neonatal care, emergency services, rehabilitation, specialty access through technology solutions, and other services, we can create new opportunities for revenue and job growth, and ultimately, we can serve the critical needs of these rural communities.
The area of Southern Appalachia served by Ballad Health serves as a case study of sorts. As an example, just last month, I met with school superintendents from throughout our region. Many of these superintendents oversee rural school systems. These superintendents shared their serious concerns for students who are increasingly showing up for school in the fall with serious mental health issues, addiction, depression and suicidal tendencies. Their teachers don’t possess the skills needed to manage the serious issues these students come to school with, and the school systems in rural areas certainly lack the resources to manage this problem on their own. Given the distant nature of the hospitals throughout the region, and the location of the schools, there is no easy solution, but there is a solution. The combination of the use of technology for assessment of these kids by qualified counselors who may not even live in those communities with the resources of the rural hospital to offer competent crisis services with a bridge to treatment makes perfect sense. But the payment system doesn’t lend itself to supporting these costs or this model for rural communities.
This is where Ballad Health, and its unique model, can be a bridge as the larger rural health policies evolve. The vast majority of the 29 counties Ballad Health serves have flat or negative population growth. Our hospitals are also experiencing above-average declines in inpatient utilization rates. Sixty-seven percent of our payor mix is Medicare or Medicaid and another six percent is self-pay. The fastest growing segment of our patients who are not paying are those who have insurance but cannot pay the higher deductibles. In addition, just as rural Americans are older and sicker than their urban counterparts, they also suffer higher rates of chronic disease such as heart disease, diabetes, obesity, substance use disorder, and untreated mental illness. Given the higher incidence of chronic conditions that make pregnancy more challenging in rural areas, it follows that rates of complications and maternal/infant deaths are higher, too. In 1985, 24 percent of rural counties lacked obstetric services. Today, 54 percent of rural counties lack hospital-based obstetric services. More than 200 rural maternity programs closed between 2004 and 2014. All of these issues are faced by Ballad Health and the rural communities we serve.
While rural populations account for only about 20 percent of our nation’s population, they populate 97 percent of our nation’s land area. In some regions, this land mass is complicated by the significant geographic barriers and distance that make the provision of services even more difficult.
These are some of the reasons our community leadership came together to create a new model of healthcare delivery. Formed only eight months ago by the merger of two competing health systems serving the same region for many decades, Ballad Health represents a transformation in the way we are approaching these challenges in our part of the country.
Both legacy systems came to recognize that our status quo was no longer sustainable. While we separately invested millions of dollars in services and technologies designed to compete with the system down the road, our community was becoming less healthy, and our margins still continued to decline. We each recognized obtaining synergies of increased scale was imperative, yet selling our systems to larger outside hospital companies or systems would have likely resulted in the closure of some rural hospitals, the devastating loss of at least 1,000 back-office jobs in our region, and as studies have shown happens, the larger systems would have likely increased pricing as they sought to leverage their size in negotiations with insurers and government payors.
Unfortunately, federal anti-trust policy in health care is solely focused on preserving competition, with little or no room to consider the effects of market failure on health and economic conditions in communities such as ours. Without this merger under state action immunity laws in Tennessee and Virginia, the hit to our region’s economic stability would have been severe.
Instead, we have begun the process of reducing resources tied up in destructive and costly duplication. We are redirecting at least $300 million of these savings to preserve essential services and to invest in initiatives that reach further upstream of the emergency department or the doctor’s office to help address the social determinants that are contributing to our region’s poor health status.
Our efforts are an attempt to build a bridge to the future of rural health care, but we will only succeed long-term if federal and state policies support what we are trying to do. While other rural hospitals are closing, we have pledged to preserve our rural hospital facilities and to repurpose many of them so that additional essential services can be provided to our community.
Referencing the conversation I had with our school superintendents, because Ballad Health retained its local governance and is a community-based organization, we decided to become a solution to the problem. Ballad Health intends to invest in counselors at our region’s only children’s hospital to do assessments of children in our schools in crisis. We plan to hire a counselor in each school district to serve those children identified with serious crisis needs. Unfortunately, the current payment system does not sufficiently support this model, but our commitment to the community is more important than profits. Eventually, the business model must support what we are investing in, and that’s why I’m here today. This is an example where a system approach to genuinely improving healthcare services can benefit the communities in the region we serve, and we hope to show this is a model worth investing in. We would welcome a federal investment into this model of partnership between rural schools and hospitals as we demonstrate how it can help solve many of our region’s problems.
Of course, this model relies upon our ability to attract and retain a high-quality and dedicated healthcare workforce. Seventy-seven percent of counties in our country are considered Health Professional Shortage Areas by the National Rural Health Association, and we are impacted by this as well. Our children’s hospital struggles to attract and retain physician talent, and we are the only children’s hospital within a two-hour drive of many residents in our region. Again, a payment system that only rewards hospital admissions does not contribute to a successful healthcare delivery system in a region where admissions are declining. Instead, federal and state policies should align to invest in needed services for underserved areas with an eye toward evolving existing facilities into centers of excellence for rural health care. I imagine a day when our children’s hospital can serve children who are developmentally disabled or suffer from mental health or other behavioral challenges, and can participate in the type of research that will help solve future healthcare problems in rural areas. Our children’s hospital has seen a rate of neonatal abstinence syndrome approximately four times greater than the national average, and we do not fully know what the impact of this will be on these children as they grow. Rural America is at the center of this problem. While urban communities typically have the depth and breadth of specialties necessary to address the issues in those communities and the research strength to obtain the funding required to study these issues, rural areas simply cannot sufficiently compete and participate.
Because of the new model we have created and are funding, our region may receive a short reprieve, but many communities are unlikely to be as fortunate. According to the Chartis Center for Rural Health, 40 percent of rural hospitals had negative operating margins in 2017, and this same study found that 44 percent of rural hospitals will have negative operating margins in 2018. Consistent with this trend, six of Ballad Health’s 14 rural hospitals had negative operating margins in the fiscal year that just ended, in addition to two of our non-urban hospitals. We continue to subsidize these losses as we build toward the future. On top of this, Ballad Health provided more than $300 million in uncompensated care last year, leading to a system-wide operating margin of only 0.6 percent, or $12 million.
Given these realities, I applaud the members of this committee for their continued leadership and efforts to facilitate passage of a comprehensive rural health care package before the end of the 115th Congress.
Simply put, rural hospitals and physicians need a federal regulatory and reimbursement environment that takes into consideration the unique circumstances faced by the hospitals and physicians serving the 20 percent of our population that lives in 97 percent of our country’s geography. As this committee considers a number of weighty issues related to health in rural areas, I would urge our policymakers to fundamentally reframe the way we think about rural hospitals and their role in their communities in two key ways.
First, we should stop thinking about rural health services in terms of bricks-and-mortar facilities and start thinking in terms of the real health problems that need to be solved in these communities. The National Rural Health Association confirms that rural Americans suffer disproportionately from serious health issues like diabetes and heart disease, and they are disproportionately more likely to die from curable cancers or drug overdose. These are not problems that can easily be solved within a traditional brick-and-mortar inpatient hospital, nor can they easily be solved within our country’s current payment system.
If we want to make a real impact on improving the health of Americans in rural areas, we need to identify the health services that are needed in those areas and then incentivize hospitals and health systems to come up with innovative solutions that fit their community’s individual needs. We need to utilize the data we have available to identify the problems and then ask the rural hospitals to come to the table with solutions. We need to identify the cost of implementing these solutions and demonstrate the potential return on investment for the payor community and the public. This can be done. While there is significant up-front investment, the potential return on investment will be undeniable.
These hospitals could benefit from renewable block funding tied to estimable costs, as opposed to the fee-for-service model that relies upon traditional service provision, to help create a bridge to what the rural hospital of tomorrow should be. This can not only help address the real problems that exist in these communities, it can create new jobs and help identify new purposes for old assets. At Ballad Health, we are in the process of doing this with two of our rural hospitals in Greene County, Tennessee. By consolidating inpatient acute care services at one hospital, we will be able to use synergies gained through our merger to repurpose the other hospital to provide the critical outpatient services, behavioral health, rehabilitation, and drug addiction treatment that are so badly needed in the community. Rather than making the easy decision to close this rural hospital, thus costing 600 jobs, we have found an alternative beneficial use for it. Given the fact that these hospitals lost a combined $11 million in 2017, and $31 million in 2016, this alternative solution, which is significantly better for the community, would only be possible within a comprehensive health system that is truly focused on the needs of the community it serves.
This brings to me the other point I would like to make about reframing our thinking about rural hospitals. Providing the proper financial incentives for rural hospitals in order to help solve population health problems can help meet the health needs of our rural communities, but this will only work if these rural hospitals are able to remain open. As you consider factors that help sustain rural hospitals, I would urge you to consider the role that many tertiary and urban hospitals within a larger, diverse health system play in sustaining the rural system of care. Many rural hospitals do not operate on their own. They are often part of larger systems that rely on the success of the regional hubs for financial viability. This is true for Ballad Health. Fourteen of our 21 hospitals are in rural areas, and six of those 14 hospitals had negative operating margins in fiscal year 2018. Were it not for the margins of our tertiary facilities, our entire rural system of care would collapse. As you consider and construct the components of a rural health package, please keep in mind that some of the non-urban hospitals with a predominantly rural health system are often a lifeline for rural hospitals, and their importance should not be overlooked.
One issue that can have a detrimental impact on both rural hospitals and the tertiary hubs that support them is the Area Wage Index. Our region of the country, like most others, suffers from a shockingly low Area Wage Index within Medicare. While our AWI is approximately 0.72, there are areas in the country with AWI in excess of 1.9. This is a zero-sum system where, despite having done employee wage increases every single year, our Medicare area wage index has continued to deteriorate, as political and other considerations have driven the wage index higher for some parts of the country. As other areas have experienced significant annual increases, ours has decreased. While the national average is supposed to be an AWI of 1.0, only 10 percent of the counties in the United States have an AWI that is greater than 1.0, while 2,600 counties have an AWI less than 1.0. This distribution is not right, and it punishes non-urban hospitals that in many cases are subsidizing the ongoing operation of rural hospitals, just as it penalizes the rural hospitals themselves. I mentioned that Ballad Health’s operating margin last year was $12 million, or a 0.6 percent margin. If there were a national floor established on the AWI of 0.874, as proposed by S.397, it would generate a $30 million annual impact for Ballad Health. In Tennessee, healthcare providers in all 95 counties and all 12 core-based statistical areas (CBSAs) are reimbursed based on AWI that are less than 0.864, which is significantly less than the national average of 1.0. I applaud the work of Chairman Alexander (R-TN), Senator Isakson (R-GA), Senator Warner (D-VA), Senator Brown (D-OH), Senator Shelby (R-AL), Senator Kaine (D-VA), Senator Roberts (R-KS), Senator Cassidy (R-LA), and Senator Jones (D-AL), many of whom are original co-sponsors of a bipartisan bill that Ballad Health encouraged be filed to help solve this problem. This bill, S.397, the Fair Medicare Hospital Payments Act of 2017, while not under the jurisdiction of this committee, would help save rural hospitals and would support the regional provision of care in non-urban America. The bill is cost-neutral and would not impact other legislative or regulatory adjustments, including the “Frontier State Fix” that established an AWI floor of 1.0 for North Dakota, South Dakota, Montana, Wyoming and Nevada. This legislation has been endorsed by the Tennessee Hospital Association, the National Rural Health Association, the Kentucky Hospital Association, the Louisiana Hospital Association, the Georgia Hospital Association, the Virginia Hospital and Healthcare Association, and the Alabama Hospital Association.
I also believe our rural hospitals could benefit from federal assistance in helping to build a bridge from the outdated fee-for-service, bricks-and-mortar model to one that is responsive to our nation’s current needs. Many rural hospitals either have debt precluding them from additional capitalization, or simply do not have sufficient resources to borrow the funds needed to build this bridge.
Modernization to right-size and reconfigure assets based on the needs of the community often needs a capital investment in order to make the transition. Community needs may include additional high-quality diagnostics, emergency medical services, outpatient rehabilitation services, mental health services, substance abuse treatment services, dentistry services, and optical health services. I would like to note that I am not advocating for simply giving away money, as I do believe rural health systems have an obligation to demonstrate the return on such investments, both financially and in terms of public health benefits. These investments would be best made in concert with effective and efficient payment reform that moves away from pay-for-volume. A Medicaid program operating in South Carolina that provides incentive payments to health systems that acquire, improve, and operate rural facilities may be a good model for Congress to consider.
I am concerned about possible policy proposals to repeal Certificate of Need requirements, which have been advocated for by some in Washington. Respectfully, I would argue that while many of us support a market-based approach, we should also acknowledge that picking and choosing the elements of the marketplace without addressing all of the necessary elements does not create a properly functioning market system. In a marketplace where more than 60 percent of care is provided in a price-prescriptive government model, private insurers reflexively copy government policies, and there is significant intrusion by both federal and state governments invoking certain mandates onto providers, it is hard to imagine anyone suggesting that the delivery of health care services exists within a free-market.
The suggestion that repealing Certificate of Need requirements in order to bring “market forces” to bear, in my view, will do more harm to our rural health system infrastructure than good. If we agree that integration of health care and better coordination would lead to better outcomes, then we must also agree that contributing to increased fragmentation in rural and non-urban communities will do harm. For instance, if Certificate of Need requirements were repealed, and a physician-owned surgery center or diagnostic center were opened in a rural community, based on current government rules and price setting, not only is there no free market, but an unlevel field has been established for competition.
Under federal law, a comprehensive hospital is not permitted to have physician ownership, and because of Stark Law regulations and anti-kickback provisions, a comprehensive hospital has very limited options for meaningfully integrating with physicians. While one competitor in the market enjoys full financial integration with physicians, including distribution of profits, which incentivizes physicians to reduce costs and increase utilization of the physician-owned facility, a comprehensive hospital is left without any such relationship. In addition, the physician-owned facility is exempt from federal EMTALA and community-benefit requirements. When one competitor has physician investment, and that competitor is not required to serve the poor, nor does it have any other obligation to help address the population health needs of the community, the local market is simply not a level-competitive market. Pulling those limited resources away from the hospital in order to provide profits to the competing physician-owned, limited-service facility only undermines that hospital’s ability to influence the other aspects of health in that community. If a rural or non-urban hospital loses its profitable services to a facility that has no obligation to help solve the mental health challenges in the region, then where will the resources come from for the rural hospital to invest in addiction care, mental health, or the other needed services? In this scenario, the hospital has been further diminished, and its survival or ability to thrive is undermined at the expense of profits for what is often an out-of-market company or financier.
I believe there are strategies that can be deployed in rural markets where the relationship between the hospitals and physicians can be strengthened. In the old fee-for-service model, Stark Law regulations and anti-kickback provisions were designed to keep financial entanglements between doctors and hospitals from affecting care. In a pay-for-value environment, those same laws inhibit the very alignment needed between doctors and hospitals to reduce unnecessary care and focus resources on prevention and chronic-care management. If the payment system were to invest in rural hospitals that convert to these models, and rural hospitals were permitted to create financial alignment with physicians, then two things will happen. First, rural communities will become more attractive to physicians who would be able to diversify their income to include the upside benefits of the hospital’s financial performance. Second, the financial and public-health success of the hospital, in alignment with the payment policies that support such a transition, would virtually ensure alignment between the physicians, hospital, and community as they seek to better manage chronic conditions, rather than simply wait until a reimbursable procedure is performed.
Please consider the following real-world example. In one community, a rural hospital has general surgeons who perform a large number of amputations, most of which are necessary due to complications from diabetes. However, that community does not have an endocrinologist. The reason many rural hospitals do not have endocrinologists is that endocrinologists do not perform procedures at hospitals, and thus, they do not generate revenue. In fact, the practice would likely lose money, in addition to the very presence of the endocrinologist reducing the need for hospitalizations, which is an outcome diametrically opposed to the financial interest of the hospital. The general surgeons will see the diabetic patients who go without management of the chronic condition, and they will perform the amputations, which are services for which the hospital and doctor get paid. In addition, the hospital does an excellent job with rehabilitation services, which again, is a service for which the hospital is paid.
However, there is an alternative: What if, noticing the high incidence of diabetes and amputations, the hospital, in a jointly established partnership with the physicians, chose to align and ask for an entirely different payment model, one that paid the hospital and physicians to invest in endocrinology services, reduce amputations, and better manage the diabetes in the population? In that scenario, better coordination occurs for the patient, the hospital and physicians may invest in technology and other innovative solutions for the management of the patients, and instead of only being paid when a procedure is performed, the hospital and physicians are compensated based on what is saved by the program.
The margins for this model would be better because the resources would be more efficiently used. This is the essence of the bundled-payments model, but I believe integration in these communities should be able to go further than the basic concept of bundled payments. Infusing flexibility into the financial relationships between physicians and hospitals can have a very positive impact on both outcomes and cost in a pay-for-value environment. It is understandable that, in a fee-for-service environment, these relationships would be problematic. However, they have been freely permitted in many areas, such as diagnostics, outpatient surgery, and others. I believe integrated models that align hospitals and physicians would open the door to many exciting opportunities to reduce cost, eliminate variation that leads to waste and poor outcomes, and create more flexible models of tackling the management of chronic illness.
These opportunities may exist, but physician alignment with hospitals must happen, and yesterday’s Stark Law regulations and anti-kickback regulations must be modernized to create these opportunities for alignment. Holding onto fee-for-service reimbursement models and preventing hospitals from more closely aligning with doctors will only preserve the outdated models that are harming rural hospitals and the health of the communities they serve.
Finally, I would like to address the need preservations of the 340B Drug Discount Program, which is a program of vital importance to the financial stability of our health system and our ability to serve vulnerable and low-income patients. While no program is free from the need for thoughtful reform, I would ask for your support in preserving 340B program eligibility for rural and non-urban hospitals as well as children’s hospitals.
We rely on these drug-acquisition savings to enable us to support the provision of care in struggling rural areas. The estimated value of the 340B program to Ballad Health in fiscal year 2019 is approximately $53 million. Again, considering the fact that our total operating margin of 0.6 percent led to only $12 million in operating surplus last year, losing access to the savings produced by participation in the 340B Drug Discount Program would be devastating for our health system and the patients and communities we serve.
Even with our participation in the 340B Drug Discount Program, Ballad Health’s annual drug spend continues to increase by over eight percent annually. Without 340B participation, our drug costs would be completely unsustainable. Reforming the 340B Drug Discount Program should not come at the cost of bankrupting vitally important hospitals and health systems. We stand with you in attempting to properly and thoughtfully reform the 340B Drug Discount Program, but we must ensure that programmatic reform does not inadvertently devastate rural hospitals and children’s hospitals across our nation.
Much of what I have presented represents a major departure from 60 years of evolution in our health system. However, I believe such major shifts in policy are important, and effective reform cannot be achieved on the margins. This is why the very creation of Ballad Health happened, and it is why our region’s major employers and every municipal government and chamber of commerce in our region encouraged and supported the merger that created Ballad Health under the doctrine of State Action Immunity from federal anti-trust law, even against the strenuous opposition by staff of the Federal Trade Commission. It is why the legislatures of the states in which we operate unanimously approved the structure of the merger under exemption from federal anti-trust law, and it is why two governors – a Democrat and a Republican – signed the legislation and authorized the merger under the advice and guidance of each state’s attorney general.
In short, there is a pent-up demand for trying something different. Ballad Health took the risk and the important step of suggesting that we want to be part of the solution rather than simply complaining about the problem. We stand ready to be a laboratory for our federal partners to help solve problems, and we stand ready to test new ways of changing the landscape of health care. Hopefully, this is just the beginning of the dialogue.
Again, I greatly appreciate the invitation and opportunity to participate in today’s hearing, and I look forward to your questions.